To explain what's new about component testing, I first have to explain what the current method of testing — enzyme immunoassay — involves. (While I do have some background in the lab sciences field, I definitely welcome any corrections from actual scientists! Leave them as comments, please.)
EIA (sometimes called ELISA), is done using plates that are preloaded with the allergenic substance into a indentation called a well. Your doctor checks off the allergens she wants tested (egg, milk, peanut, etc.) and the technician puts a sample of blood from the test patient into the well that contains the appropriate allergen. The analyzer then sends the panel through a series of chemicals and processes that encourages the antibodies in the patient's blood to bond with the purified antigen/allergenic protein (like egg) that's in the well. The extra, unneeded gunk (technical term!) is washed away and then a chemical is added to make the bonded antibodies/antigens either change colors, fluoresce (FIA) or become radioactive (RIA) so the analyzer can count them up.
The RAST (radioallergosorbent test) numbers we get back as a result is measures in kilounits per liter (kU/L), where the "unit" part is arbitrary. (One of the problems with early RAST testing is that the different analyzer manufacturers did not standardize on how they reported results, so result sets from two different analyzers could be very different.) This number is just telling us how much antibody from the patient's blood actually stuck to the plate.
The allergen extracts used in the current process are a little clunky. Laboratories extract the allergens used in the test panels from natural substances. This can be a big problem because, for example, using different varieties of apples or even a male vs. a female cat can result in variations in the amount of some proteins. The extracts are continually improved and modified, but different individuals or populations can be sensitive to different proteins, so the test is a one-size-fits-most process.
Additionally, proteins in the body and proteins in the lab don't always behave the same. For example, stomach acid can pull pieces of them apart, changing their three-dimensional shape and therefore how they bond. Other blood components (like plasma) can also alter how much antibody sticks to the plate. All of these things can contribute to false positives and false negatives on tests. That's why RAST test results have to be interpreted in conjunction with patient history and/or skin prick testing.
 |
| The "Ep" epitope areas on the protein hook up with the "Ab" antibodies, triggering the immune response. |
The enzyme immunoassay process used up until now contained ALL the appropriate epitopes because it started with a natural source. However, there was no way to tell which epitope or epitopes were causing the problem. In contrast, a component test uses a recombinant DNA process to make only a specific epitope. If the child is positive, he or she is positive only to that epitope.
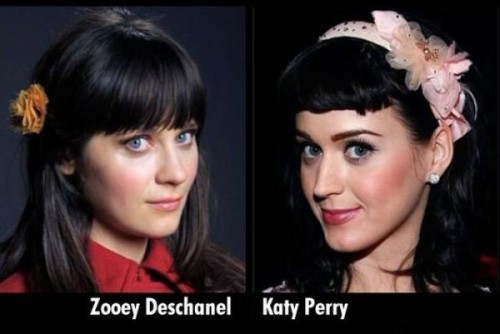 |
| Just like with faces, some bodies are better at telling proteins apart |
To give you an example, the birch protein (Bet v 1) looks like a whole lot of other proteins to the body, including those in celery, hazelnut and apple. Sometimes a primary allergy to birch pollen can cause a food allergy test to show a false positive. For many people, this cross-reaction only causes oral allergy syndrome (OAS) and their reaction never proceeds beyond an itchy mouth.
Sometimes homologues are harmless misunderstandings...and sometimes they mean a little bit more. This study from 2004 shows that up to 40% of patients sensitized to birch pollen experienced more than just an itchy mouth when they ate peanut butter, even though their peanut allergy was the result of their body thinking birch (Bet v 1) was really peanut (Ara h 8). Evil birch can also cross-react with soybean (Gly m 4).
So...the takeaway is that there's a continuum of severity of reactions when it comes to these look-alike proteins. Some are just not likely to be problematic, but with others, whether a full-out allergic reaction occurs may depend on the individual's body chemistry, how much it "looks" like the other protein and how durable the protein itself is. Knowing which protein is involved is only the first step in the process and a food challenge is still the best way to figure out if an allergy exists.
So now the question is...which epitopes cause the problems in people who are allergic? And why would knowing which epitope help us in any way to understand our child's allergy? Can we use this technology to know which allergies are life-threatening? Persistent? Interlinked, so we can predict which foods not to give our kids? Or is it just another $300 we'll never see again?
Part 2 - Why Should We Care.
Follow me on Facebook or Twitter for updates!

Our allergist indicated that the more specific test would be helpful for those who score high on RAST but don't react--they could better deduce whether reactions are ever likely to occur by using a test like this. But for a child like mine who has so many anaphylactic reactions under her belt, he didn't feel there was much of a point to it--although we don't know with 100% certainty that any of those reactions were due to peanuts, he says her general reactivity coupled with high RAST numbers makes it a no-brainer (not his words, but mine). I think it would be best for people to have a bit more certainty about whether they are truly reactive. It's like there is a spectrum of peanut reactivity, but currently everyone assumes the worst when there are any positive test results. I really wish that "mild peanut allergy" could become an accurate description for some people, and maybe that's what will happen with these tests.
ReplyDeleteVery interesting. Thank you for sharing.
ReplyDelete